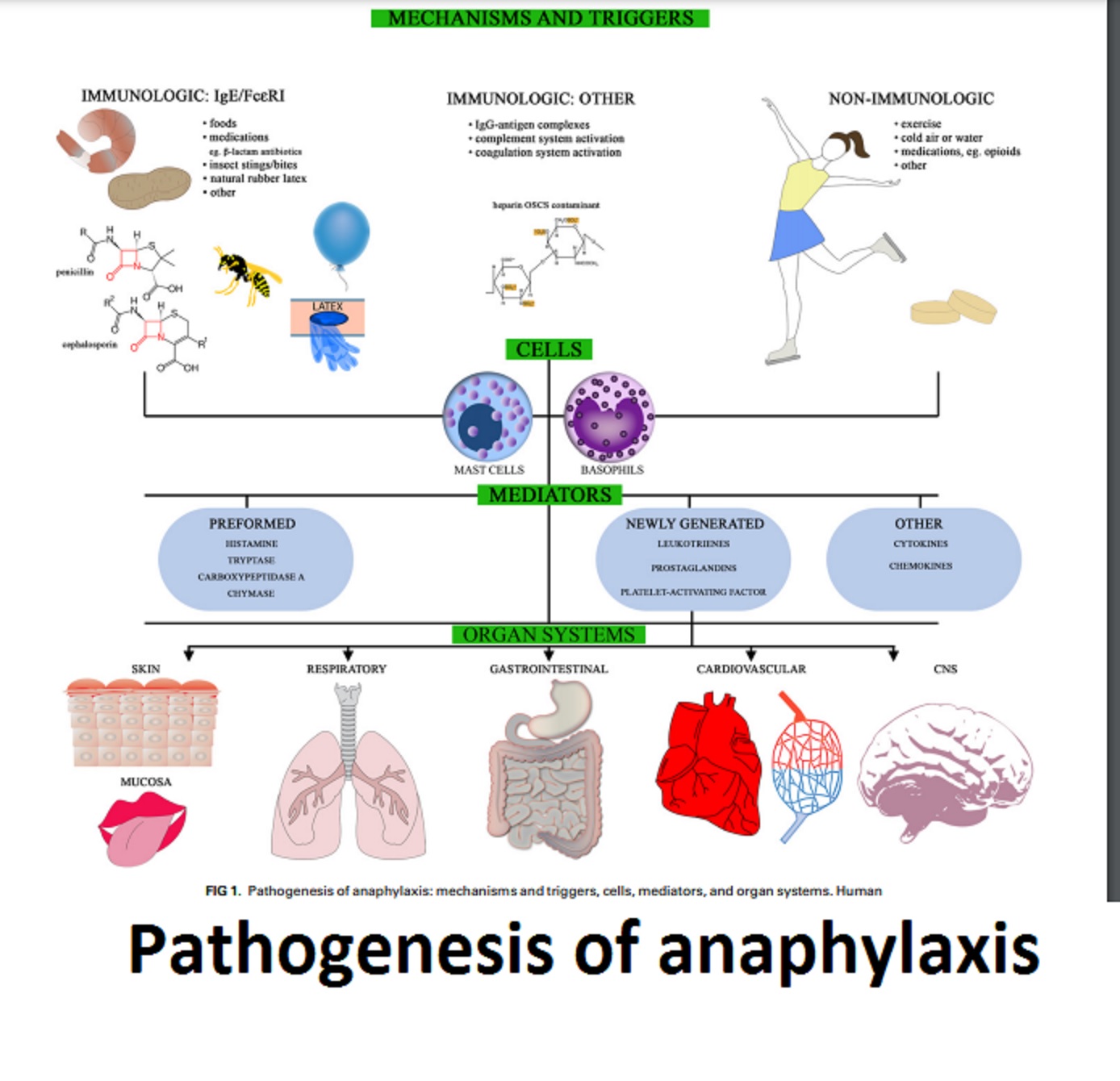
Milk allergy is a condition characterized by an adverse immune system response to proteins found in milk and dairy products. In Individuals with a milk allergy, the immune system perceives the proteins present in milk and milk-based products as potentially harmful triggering an immune response. In response, the immune system produces IgE antibodies specific to those milk proteins. The antibodies bind to specialized cells known as mast cells and basophils which are present in various tissues throughout the body particularly in the respiratory and gastrointestinal systems.
Upon subsequent exposure to milk proteins, the allergenic proteins bind to the IgE antibodies already attached to the mast cells and basophils. Consequently, the immune response prompts the release of a variety of chemical substances including inflammatory mediators like histamine among other compounds. The release of these compounds causes the symptoms associated with a milk allergy.

The prevalence of cow’s milk allergy or hypersensitivity is commonly observed to be around 2-3% in infants and 0.5-3% in adults, although these figures can vary among different populations. Allergies have a significant impact on the quality of life and health of a substantial portion of the American population. However, testing for allergies can be expensive for individuals without insurance coverage, with costs ranging from $60 to $300 for skin testing and $200 to $1,000 for blood testing.
Common Symptoms of Milk Allergy
The signs and symptoms of milk allergy can manifest in different systems of the body. Here are some common symptoms:
- Digestive symptoms: Common symptoms of milk allergy include abdominal pain, cramping, nausea, vomiting, diarrhea, a bloated or gassy sensation and in severe cases, blood in the stool.
- Skin reactions: Hives (red, raised, itchy bumps on the skin), Eczema (itchy, inflamed skin), and Swelling (angioedema), typically around the lips, face, tongue, or throat.
- Respiratory symptoms: Wheezing (a high-pitched whistling sound during breathing), coughing, shortness of breath or difficulty breathing, runny or stuffy nose and sneezing.
- Anaphylaxis: Anaphylaxis is a severe, life-threatening allergic reaction that can affect multiple systems of the body. Symptoms may include difficulty in breathing or wheezing, swelling of the lips, tongue, throat, or face, rapid or weak pulse, dizziness or lightheadedness, and loss of consciousness.
Diagnostic Process for Milk Allergy
Here’s an overview of the diagnostic process for milk allergy:
- Medical history: The healthcare provider will inquire about the individual’s symptoms and their relationship to milk consumption. Details about the timing, duration, and severity of reactions will be discussed. A thorough medical history helps establish a potential link between symptoms and milk ingestion.
- Physical examination: A physical examination may be conducted to assess visible signs of an allergic reaction such as skin manifestations like hives or eczema and to evaluate the respiratory and gastrointestinal condition.
- Elimination diet: In certain situations, the healthcare provider may recommend an elimination diet which involves the temporary removal of all milk and dairy sources from the individual’s dietary intake. If symptoms resolve during this elimination period and return upon reintroduction of milk, it may indicate a milk allergy.
Diagnostic tests:
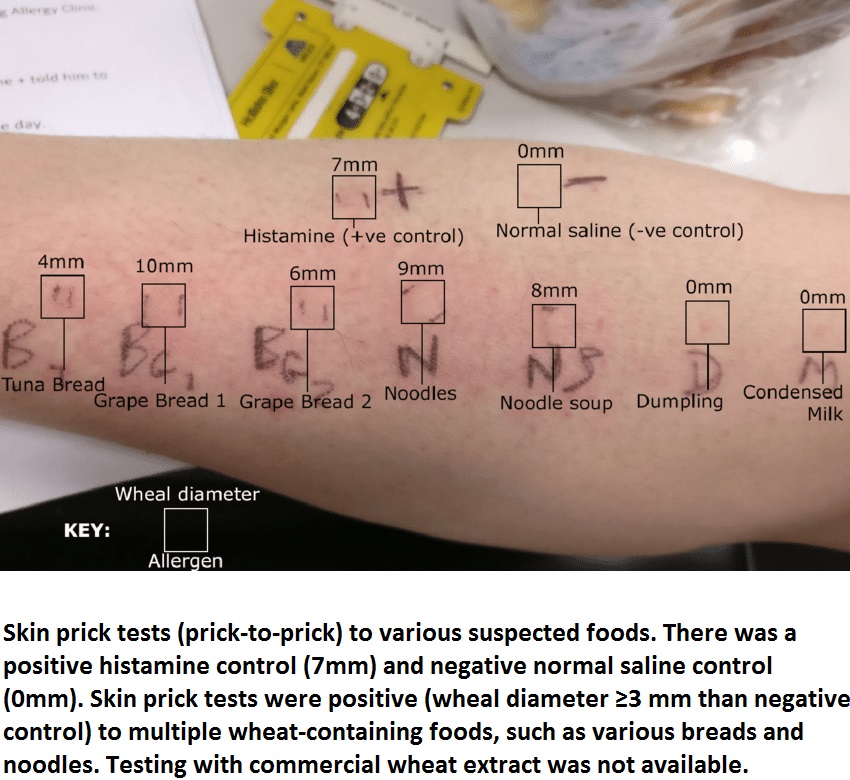
- Skin prick test: This test involves placing a small amount of milk protein extract on the skin, usually on the forearm or back, and gently pricking or scratching the surface. If the individual is allergic to milk, a small raised bump (wheal) surrounded by redness (flare) may develop at the test site.
- Blood tests: Blood tests can measure specific IgE antibodies to milk proteins. The diagnosis of milk allergy often entails two types of blood tests: the specific IgE and the allergen component test. These tests help determine the presence and level of milk-specific antibodies in the blood.
Understanding Milk Allergens: Casein and Whey
Milk contains several proteins that can trigger allergic reactions in individuals with milk allergies. The two primary proteins for most milk allergy are casein and whey.
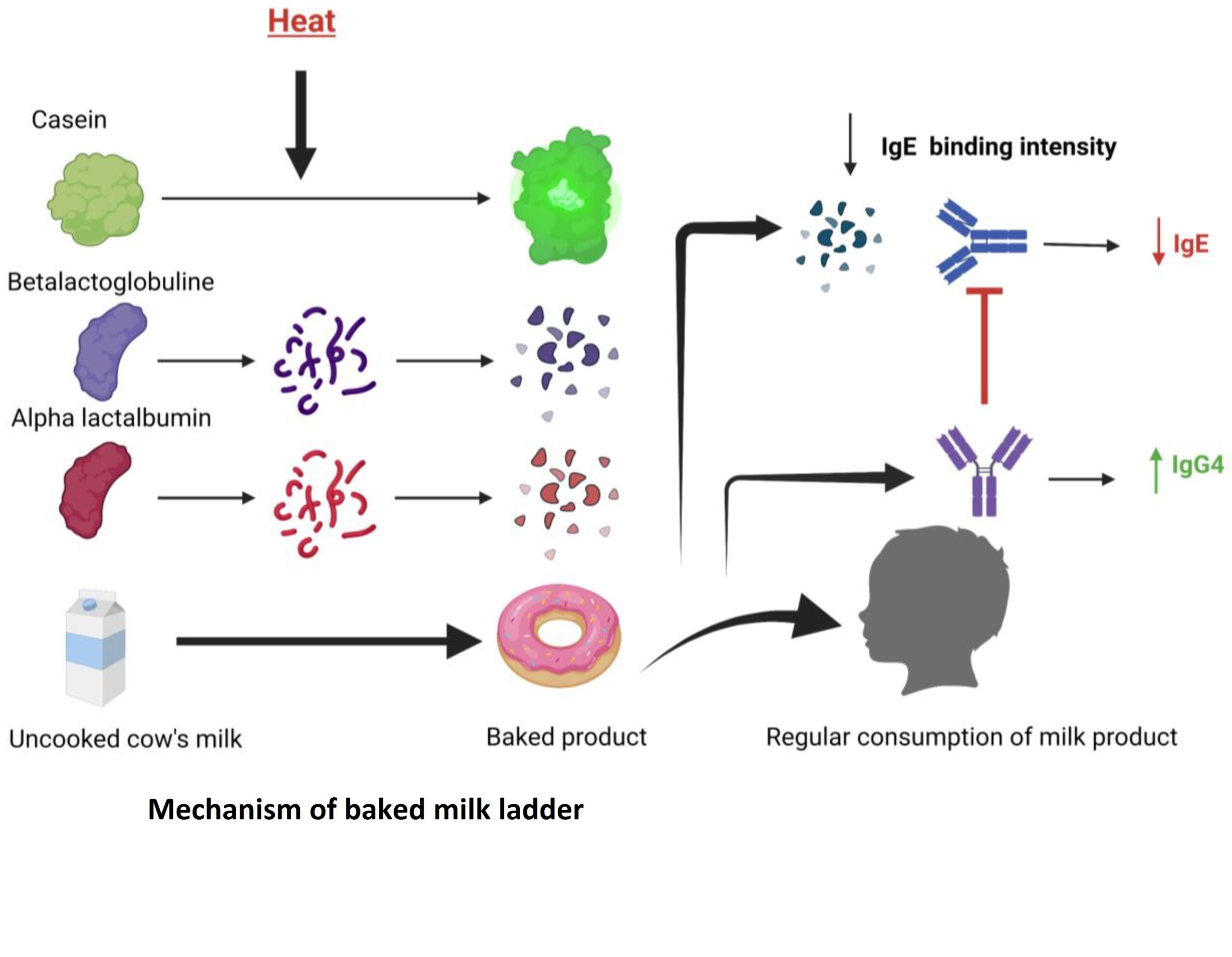
- Casein: The major protein found in milk accounting for around 80% of the total protein content is known as casein and represents the primary protein component in milk. It is a complex protein that consists of various subtypes, including alpha-casein, beta-casein, and kappa-casein. Some individuals with milk allergy may react specifically to one or more of these casein subtypes.
- Whey: Whey protein makes up approximately 20% of the total protein in milk. It is composed of various proteins with beta-lactoglobulin and alpha-lactalbumin being the primary protein components. These proteins can trigger allergic reactions to milk.
Both casein and whey proteins are capable of eliciting an immune response in individuals with milk allergy. The immune system recognizes specific epitopes (parts) of these proteins as foreign and launches an allergic response, producing antibodies such as IgE.
It’s worth noting that there are other minor proteins present in milk, such as lactoferrin, lactoperoxidase, and immunoglobulins, but they do not typically play a significant role in milk allergy.
Cross-Reactivity and Hidden Sources of Milk in Milk Allergy
Cross-reactivity and hidden sources of milk are important considerations for individuals with milk allergies. Here are some key points:
- Cross-reactivity: Individuals with milk allergy may experience cross-reactivity with other allergens, particularly proteins that share similar structures with milk proteins. Common cross-reactive allergens include those found in other mammalian milk (e.g., goat, sheep), beef, and soy. Cross-reactivity can lead to allergic reactions when consuming these cross-reactive foods, even if they do not contain milk proteins directly. It is crucial to remain mindful of these potential cross-reactivities and seek guidance from a health care professional or allergist to ensure appropriate management.
- Hidden sources of milk: Milk and its derivatives are present in a diverse array of food products including baked goods, processed foods and even non-edible items like medications or cosmetics. Food labels may use terms such as casein, whey, lactoglobulin, lactalbumin, or ingredients derived from milk like butter, cream, or cheese. It’s crucial to carefully read ingredient labels to identify hidden sources of milk. Some processed foods may also have the advisory statement “May contain milk” or “Processed in a facility that also processes milk,” indicating a potential risk of cross-contamination. Skim milk and buttermilk are milk variants with different fat content, while chocolate is a popular flavored milk product.
Challenges of Milk Allergy in Daily Life
- Dietary restrictions: Strictly avoid milk and milk-based products and seek alternative dairy-free options.
- Social situations: Communicating dietary restrictions, bringing own food to social gatherings, and navigating parties or events with potential milk-containing dishes.
- Dining out: Informing restaurant staff, inquiring about ingredients and cross-contamination risks, and choosing allergen-friendly establishments.
- School and childcare: Establishing protocols, communicating with teachers and caregivers, and educating others about the allergy.
- Travel and food labeling variations: Researching local food customs, carrying allergy translation cards, and being prepared with safe snacks while traveling.
- Emotional impact: Dealing with constant vigilance, potential anxiety, and the need for support from healthcare professionals and loved ones.
Non-Dairy Sources for Essential Nutrients
For individuals with milk allergies, obtaining essential nutrients typically found in milk is still possible through non-dairy options. Here are some alternative sources for key nutrients:
Calcium:
- Leafy green vegetables like kale, broccoli, and spinach.
- Fortified plant-based milk such as almond milk, soy milk, rice milk.
- Tofu made with calcium sulfate.
- Canned fish with soft, edible bones including salmon and sardines.
Vitamin D:
- Sunlight exposure (15-20 minutes a day)
- Fortified plant-based kinds of milk, orange juice, and cereals
- Fatty fish (e.g., salmon, mackerel)
- Mushrooms exposed to UV light
Protein:
- Legumes (beans, lentils, chickpeas)
- Quinoa
- Nuts and seeds (almonds, chia seeds, hemp seeds)
- Tofu and tempeh
- Plant-based protein powders (pea protein, brown rice protein)
Managing Milk Allergy in Children
Addressing milk allergy in children requires careful management to ensure they receive proper nutrition. Here are key considerations:
- Breastfeeding considerations: When a breastfed baby experiences a milk allergy, it may require the mother to exclude dairy products from her own diet. Seeking guidance from a healthcare professional or allergist is recommended to ensure proper nutrition for both the mother and baby while effectively managing any potential allergic issues. Breast milk substitutes may be suggested if complete dairy elimination is challenging or if symptoms persist.
- Formula options: Specialized hypoallergenic formulas, such as extensively hydrolyzed formulas or amino acid-based formulas, are available for infants with milk allergies. These formulas have proteins broken down into smaller fragments or contain amino acids, minimizing the risk of allergic reactions. It is essential to consult with a healthcare professional when selecting an appropriate formula, as they can assess factors such as the child’s age, the severity of the allergy and individual requirements to make an informed decision.
- Managing the allergy as they grow: As children grow, monitoring for hidden sources of milk and cross-contamination becomes important during the introduction of solid foods. Regular follow-up with healthcare professionals helps assess growth and adjust the diet accordingly. Educating caregivers and school staff, along with consulting a registered dietitian, ensures alternative nutrient sources and monitoring for potential deficiencies.
Support Resources for Milk Allergy
There are several resources available to support individuals with milk allergies and provide guidance for managing the condition. Here are some helpful sources:
- Allergy Organizations:
Food Allergy Research & Education (FARE): FARE provides resources, support, and educational materials for individuals with food allergies, including milk allergies. Their website offers practical tips, research updates, and a community forum.
The American Academy of Allergy, Asthma & Immunology (AAAAI): The AAAAI (American Academy of Allergy, Asthma & Immunology) provides resources and information regarding allergies and allergic conditions including milk allergy. Their website provides access to articles, guidelines, and a directory of allergists.
- Online Communities And Forums:
Allergic Living Forum: Through this online forum, individuals with allergies along with their families can come together exchange personal experiences and seek guidance from others facing similar circumstances.
Health Unlocked: Health Unlocked hosts various allergy-related communities, where individuals can ask questions, share stories, and find support.
- Social Media Groups:
Facebook groups: There are numerous Facebook groups dedicated to supporting individuals with food allergies, including milk allergies. Examples include “Parents of Kids with Food Allergies” and “Living with Milk Allergy Support Group.”
Instagram: On Instagram, hashtags like #milkallergy, #dairyfree, and #foodallergylife can lead to finding accounts and communities sharing information and support related to milk allergy.
Local support groups: Local allergist offices or hospitals may host support groups or be able to provide information about local resources and community gatherings for individuals with milk allergies.
Emergency Preparedness: Allergies, EpiPens and Action Plans
Having an emergency action plan is crucial for individuals with severe allergies, outlining specific steps during an allergic reaction. It is crucial to have prescribes epinephrine auto-injectors like Epipens readily available at all times as they serve as the primary intervention for anaphylaxis effectively counteracting severe allergic reactions. These measures ensure preparedness and prompt response to allergic emergencies. Prompt administration of epinephrine can be life-saving during an allergic emergency.
Advancing Milk Allergy Treatment: Ongoing Research and Future Therapies
- Oral Immunotherapy (OIT): Oral immunotherapy is a promising approach currently being studied for milk allergy. This therapy consists of a gradual introduction of small quantities of milk protein to individuals aiming to desensitize their immune systems and minimize allergic reactions. Research studies have shown that OIT can increase milk tolerance in some individuals, allowing them to consume small amounts of milk without severe allergic reactions. OIT (Oral Immunotherapy) is currently in the experimental phase and should only be undertaken with the guidance and supervision of healthcare professionals.
- Sublingual Immunotherapy (SLIT): Similar to OIT, sublingual immunotherapy aims to desensitize the immune system by administering milk allergens under the tongue. This therapy is less invasive than OIT since it doesn’t involve swallowing the allergen. While some studies have demonstrated encouraging outcomes in enhancing milk tolerance with SLIT, further research is necessary to ascertain its long-term effectiveness and safety.
- Epicutaneous Immunotherapy (EPIT): Epicutaneous immunotherapy involves applying small amounts of milk allergens to the skin using a patch. The allergens are absorbed through the skin, aiming to induce desensitization. Recent clinical trials have reported encouraging findings indicating enhanced milk tolerance and decreased allergic reactions in children diagnosed with milk allergies. EPIT (Epicutaneous Immunotherapy) is regarded as a non-invasive and potentially safer alternative to other forms of immunotherapy. However, additional research is necessary to conclusively determine the effectiveness and long-term outcomes of the treatment.
- Allergen-Specific Immunoglobulin E (IgE) Inhibitors: Researchers are exploring the use of allergen-specific IgE inhibitors as a potential treatment for milk allergy. These inhibitors target and neutralize the specific IgE antibodies responsible for allergic reactions.
Clinical trials are currently being conducted to assess the efficacy of this approach presenting a promising possibility for a focused and specialized treatment alternative for individuals with milk allergy.
Novel Therapies and Biologics:
Several other novel therapies and biologics are being investigated for the treatment of milk allergy. These include monoclonal antibodies targeting specific immune cells or molecules involved in the allergic response. Furthermore, scientists are investigating the potential benefits of probiotics, prebiotics and other immune-modulating strategies in the management of milk allergy.
Outgrowing Milk Allergy: Importance of Re-evaluation with an Allergist
- Many children may outgrow milk allergy, but it varies by individual.
- Re-evaluation with an allergist is crucial to determine if the allergy has been outgrown.
- An allergist conducts tests and assessments to assess the current status of the allergy.
- Re-evaluation ensures accurate diagnosis, monitors progress, and provides guidance on dietary management.
- Early detection of outgrowing allows for the reintroduction of milk products, improving quality of life.
- Re-evaluation prevents unnecessary dietary restrictions.
Some Common Questions On Milk Allergy
Is milk allergy a lifelong condition?
Milk allergy is typically not a lifelong condition, as many children may outgrow it over time, but it can persist into adulthood in some cases.
Can milk allergy lead to other food allergies?
Having a milk allergy can increase the risk of developing other food allergies, as individuals with milk allergies are more likely to be allergic to other common allergenic foods such as eggs, soy, and peanuts.
What are the emotional and psychological impacts of living with milk allergy?
Living with milk allergy can lead to emotional and psychological impacts such as anxiety, social isolation, and feelings of exclusion, as individuals may face challenges navigating social situations, dietary restrictions, and potential allergen exposures.
Can individuals with milk allergies consume other dairy products like cheese or yogurt?
Individuals with milk allergies must avoid all dairy products, including cheese and yogurt, as they are derived from milk and contain milk proteins that can trigger allergic reactions.
How is milk allergy different from lactose intolerance?
Milk allergy is an immune response to proteins in milk, while lactose intolerance is the inability to digest lactose, the sugar found in milk, due to insufficient lactase enzyme.
Can exercise trigger or worsen milk allergy symptoms?
Exercise itself does not directly trigger or worsen milk allergy symptoms. However, strenuous exercise can sometimes cause symptoms that may be mistaken for an allergic reaction, such as shortness of breath or hives. If these symptoms occur during exercise, it is important to stop the activity and seek medical attention to determine the cause.